Blue Cross Blue Shield Of Mississippi Prior Authorization Form - All disease specific drugs must be prescribed by a network provider, prior authorized by blue. If you are a mississippi network provider, you should submit your prior authorization requests. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Prior authorization status please start the request by providing the following provider and patient. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and.
All disease specific drugs must be prescribed by a network provider, prior authorized by blue. If you are a mississippi network provider, you should submit your prior authorization requests. Prior authorization status please start the request by providing the following provider and patient. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires.
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Prior authorization status please start the request by providing the following provider and patient. If you are a mississippi network provider, you should submit your prior authorization requests. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and.
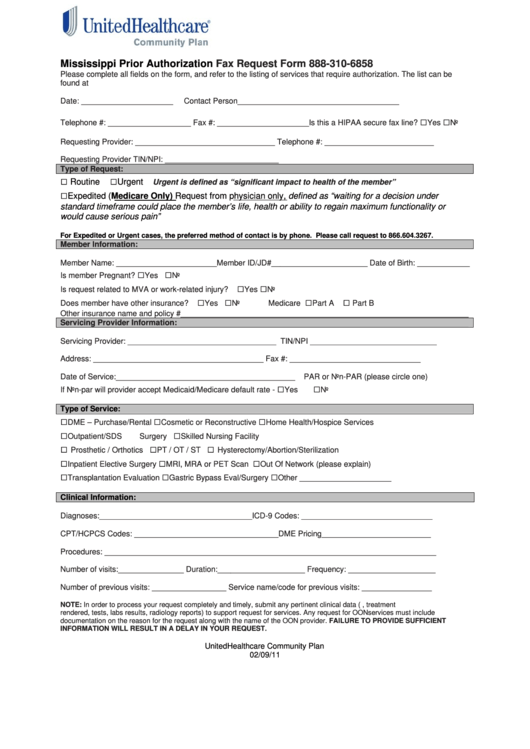
Fillable Mississippi Prior Authorization Fax Request Form printable pdf
All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. If you are a mississippi network provider, you should submit your prior authorization requests. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Prior authorization status please.
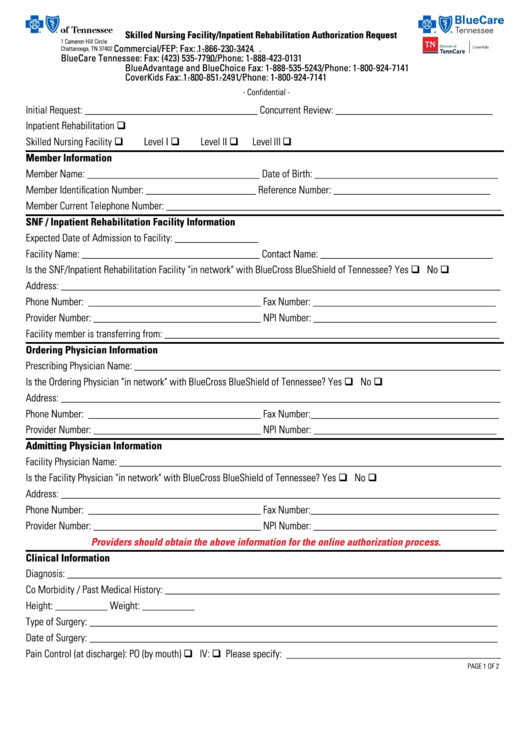
Fillable Online Blue cross blue shield prior authorization form pdf Fax
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Prior authorization status please start the request by providing the following provider and patient. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. If you are a.
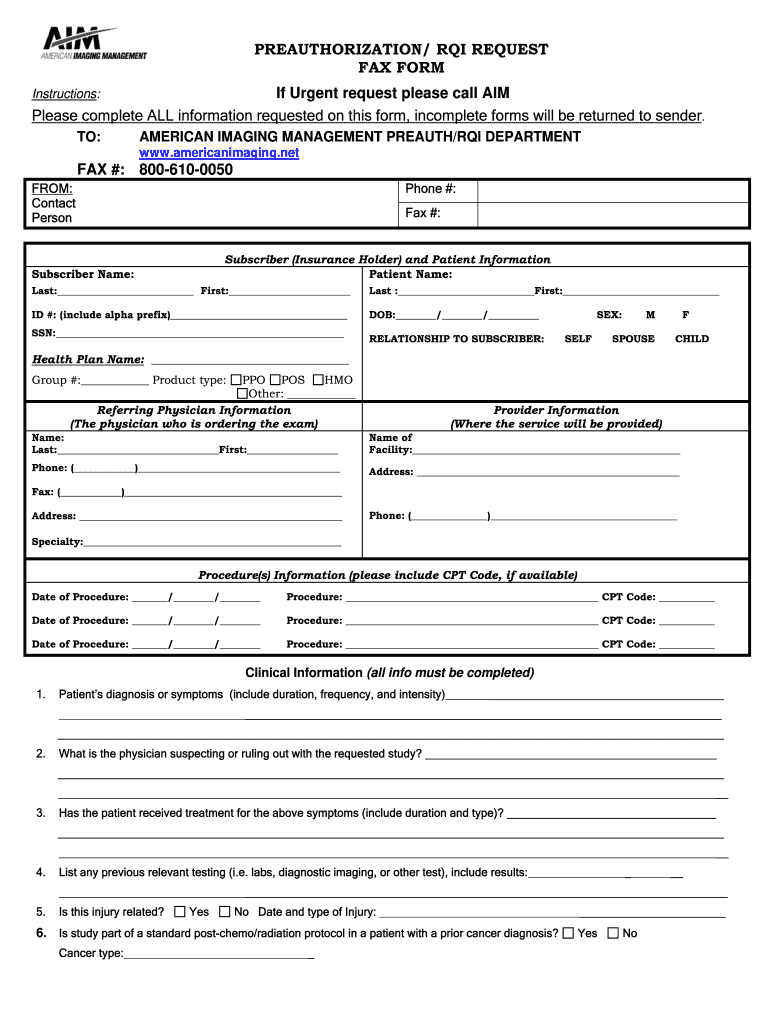
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates free
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Prior authorization status please start the request by providing the following provider and patient. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. If you are a.
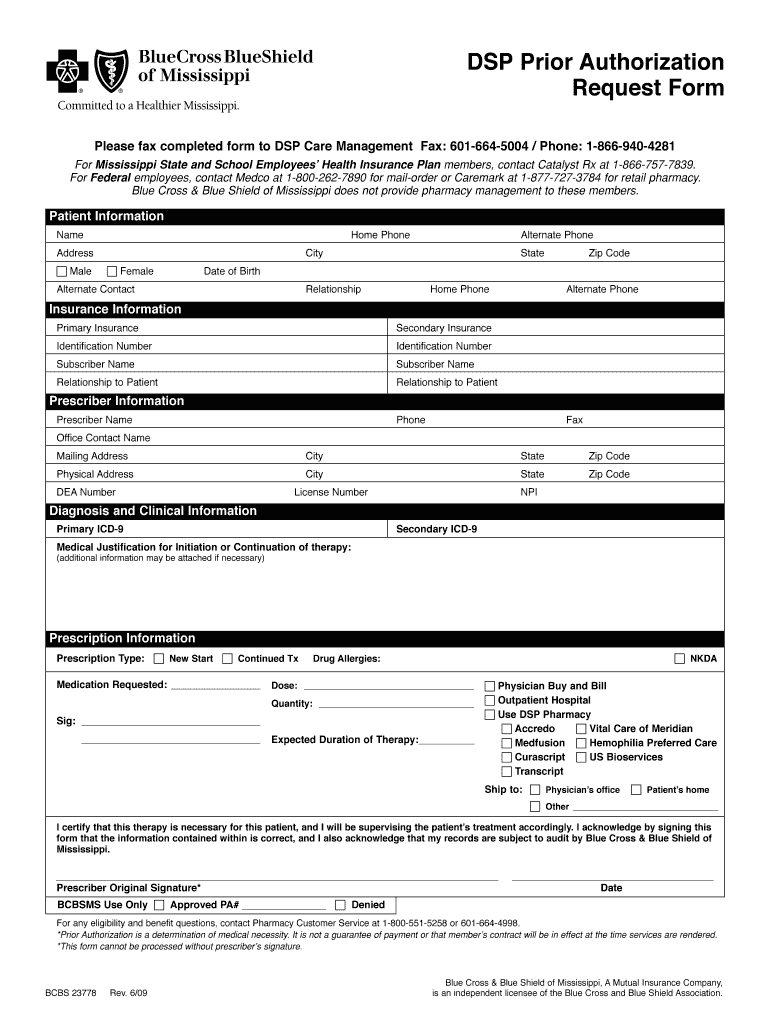
Bcbs mississippi Fill out & sign online DocHub
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Prior authorization status please start the request by providing the following provider and patient. If you are a mississippi network provider, you should submit your prior authorization requests. Certain drugs must be prior.
Mississippi Bluecross Form Fill Online, Printable, Fillable, Blank
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prior authorization status please start the request by providing the following provider and patient. If you are a mississippi network provider, you should submit your prior authorization requests. All disease specific drugs must.
Blue Cross Blue Shield Of Massachusetts Prior Authorization Form
All disease specific drugs must be prescribed by a network provider, prior authorized by blue. If you are a mississippi network provider, you should submit your prior authorization requests. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prior authorization status please.
Blue Cross Blue Shield Sleep Study Authorization Form Study Poster
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prior authorization status please start the request by providing the following provider and patient. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. If you are a mississippi network provider, you should submit your prior authorization requests. All disease specific drugs must.
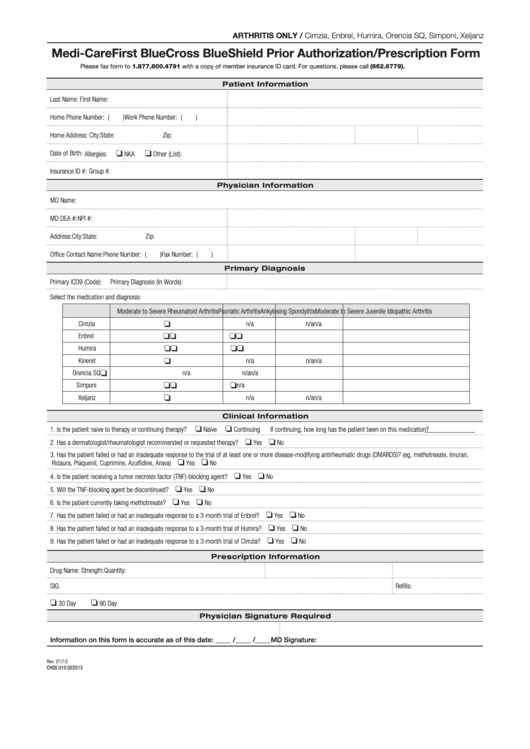
Fillable Medicare First Blue Cross Blue Shield Prior Authorization
If you are a mississippi network provider, you should submit your prior authorization requests. Prior authorization status please start the request by providing the following provider and patient. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. All disease specific drugs must.
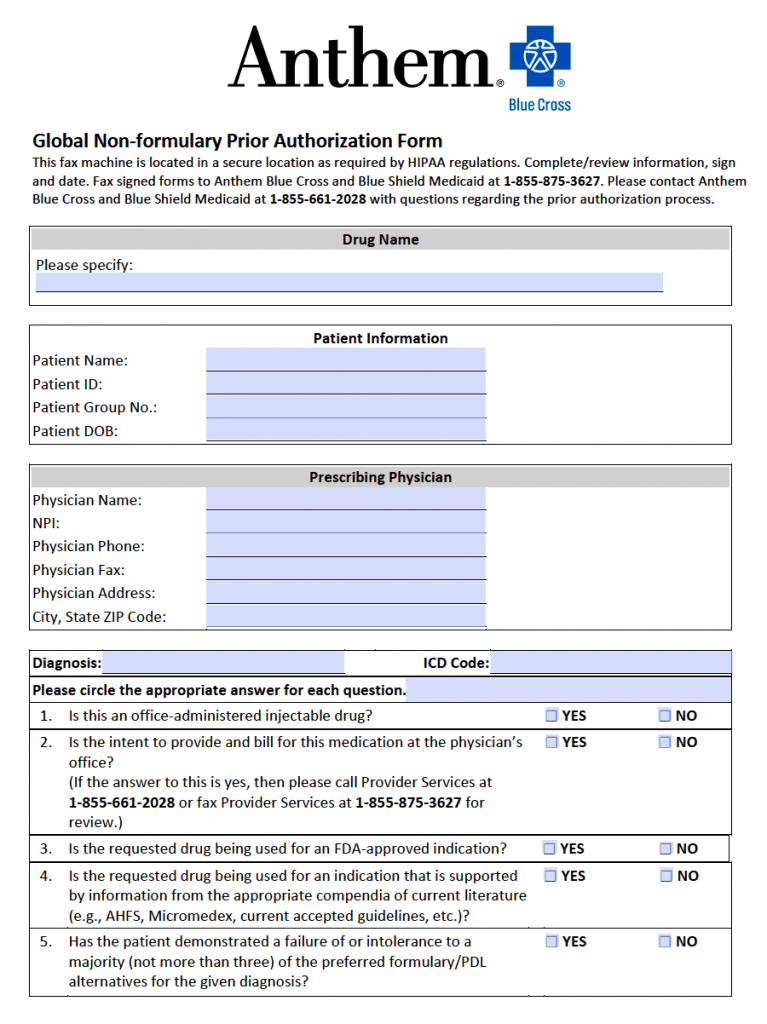
Free Anthem Blue Cross / Blue Shield Prior Prescription (Rx
If you are a mississippi network provider, you should submit your prior authorization requests. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. Prior authorization status please.
CA Blue Shield Prior Authorization Request Form Resonance
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Prior authorization status please start the request by providing the following provider and patient. If you are a.
Prior Authorization Status Please Start The Request By Providing The Following Provider And Patient.
If you are a mississippi network provider, you should submit your prior authorization requests. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and. All disease specific drugs must be prescribed by a network provider, prior authorized by blue. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires.